Reduziere Neurodermitis
mit Sanubiom SkinCare Protect mit Phage Technology
Atopic dermatitis is the most common chronic disease in babies and children. This inflammatory skin disease is also known as atopic dermatitis or atopic eczema.
Many babies and children are affected by this agonizing itching. The number of cases has tripled in recent decades.
Find out here how you can prevent atopic eczema in your child and treat atopic dermatitis in babies at an early stage. With this knowledge, you can enable your child to live a life free of complaints.
Around 13 percent of schoolchildren are affected. As a rule, the first skin eczema appears before the age of five. In half of all young patients, atopic dermatitis even manifests itself in the first 6 months of life.
The manifestations of atopic dermatitis depend on age. Both the localization of eczema and the severity of the symptoms of atopic dermatitis in infants and small children differ from those in adults.
In a child, for example, the conspicuous patches of skin and redness mainly appear on the head, while the disease can spread to the entire body as it progresses.
The agonizing itching is often particularly stressful for the affected children and sometimes triggers regular scratching attacks.
Children whose parents suffer from allergies are particularly at risk of falling ill. Sometimes the inflammatory skin disease disappears as the child grows up. In other cases, it persists into adulthood.
Read here what you need to know about atopic dermatitis in babies and children in order to understand, recognize and treat it at an early stage. With this knowledge, you can enable your child to live a life free of complaints.

Atopic dermatitis is the most common chronic skin disease in children. It can manifest itself as dry skin, severe itching, redness or even weeping eczema.
There is no causal therapy to date. But with the help of good basic care, atopic dermatitis can be treated even in small children. There is therefore a chance that the symptoms of atopic dermatitis will only develop to a lesser extent and disappear completely over time.
Even though it is always intermittent and chronic, atopic dermatitis in babies and young children differs from the disease in other age groups.
Recognizing atopic dermatitis in babies is important for correct treatment and successful and rapid relief of the symptoms.
Neurodermatitis often occurs as early as the second or third month of life and babies cannot yet tell us exactly what is wrong with them.
However, there are some signs by which you can recognize typical symptoms of atopic dermatitis.

Atopic dermatitis in babies usually starts on the face, the crooks of the arms and knees and the hairy part of the head. Initially, inflamed areas of skin develop, which can ooze and form crusts.
This early stage on the head is also known as cradle cap. As the disease progresses, such foci of inflammation also develop in other parts of the body, especially on the arms and legs.
The diaper region is usually not affected. A double eyelid crease under the eyes can also indicate atopic dermatitis.
This so-called “Dennie Morgan fold” is particularly noticeable in babies.
Together with other symptoms, however, it can contribute to a clear diagnosis.
In small children, the typical neurodermatitis symptoms are very often found in the bends of the joints, such as the elbows, knees and wrists.
This is referred to as flexural eczema. These usually cause terrible itching and severe redness.
The neck, buttocks and thighs, as well as the backs of the feet and hands of small children can also show inflammatory skin changes.
Children who suck their thumbs are often also affected.

Atopic dermatitis in children typically begins between the age of two and puberty.
At the beginning, parents usually only notice the extremely dry skin of their children. However, itchy, scaly areas and redness develop quite quickly. After a prolonged course, the sensitive skin can become uneven, thickened and leathery.
Unlike babies, cradle cap no longer occurs at this age. Instead, it typically affects the bends of the joints, the neck, the hands and the folds between the buttocks and ankles.
Special forms of atopic dermatitis are so-called sucking eczema around the mouth, eyelid eczema and hand and foot eczema, the so-called “winter feet“.
Not every skin irritation has to be atopic dermatitis. However, if you notice skin changes in your child, it is important to sharpen your senses and observe the development of symptoms over a longer period of time in order to recognize possible atopic dermatitis.
Are you affected by atopic dermatitis yourself or do you have a family history of it? Is your child constantly scratching or complaining of severe itching? Does the eczema not disappear with simple skin care, but remain present for a longer period of time?
Then a disease with neurodermatitis is very likely. It is best to consult a pediatrician or dermatologist to clarify the suspicion and discuss possible treatment.
With young children in particular, it is possible that the symptoms of atopic eczema will subside over time if treatment is started early.


After birth, the newborn initially has a natural skin protection, the so-called cheese gunk.
This is a light-colored secretion of dead horny cells and fat that protects the baby’s skin in the amniotic fluid.
The antibacterial substances it contains protect the baby from infections during or immediately after birth.
The cheese smear is gently removed from the newborn. After that, parents should take over the care of the baby’s skin.
The skin of a newborn baby is not yet fully developed. It is much thinner than the skin of adults and therefore not as resistant.
The protective functions of baby skin must first mature. This means that the barrier is not yet stable and the baby’s skin is much more permeable, so that it loses moisture very quickly and dries out.
In addition, allergens and irritants that come into contact with the skin are absorbed more quickly and can penetrate more easily.
This also applies to pathogens and germs. If there is also a genetic predisposition to atopic eczema, it is almost guaranteed that the offspring will also react to certain triggers and neurodermatitis symptoms will occur.
Incidentally, babies’ facial skin is even thinner than the skin on the rest of the body, which is why atopic dermatitis in babies first appears on the head.
According to a study, there is a direct link between our modern diet and atopic dermatitis.
According to the report, the proportion of meat and animal fats in our diet is increasing, while less fish with omega-3 fatty acids and antioxidants in fruit and vegetables are on the menu. This unbalanced diet is causing more and more people to suffer from atopic dermatitis.1
In addition, many foods are suspected of worsening existing atopic dermatitis in small children. The list of suspect foods includes:
However, as the tolerance of certain foods varies from person to person, there is no universal nutritional therapy for neurodermatitis patients.
What leads to successful treatment for one person may even worsen the clinical picture for another.
It is often helpful to keep a food diary to identify the triggers of acute flare-ups of atopic dermatitis.
In this way, allergic reactions caused by food can be identified and the correct personal diet for neurodermatitis can be adapted accordingly.
In general, however, food is often difficult to prove as a trigger for neurodermatitis flare-ups.
The resulting fears and stress reactions are usually more worrying than the suspected substances themselves.

You can treat your child’s atopic dermatitis symptoms with targeted measures. Dryness, redness, cracking and thickening are alleviated. The risk of infection is reduced, significantly minimizing the emotional strain on the entire family.
A study by Dr. Hanna Hill also reviewed allergen testing data to identify the most common contact allergens in children. She found that certain ingredients in nasal sprays, shampoos and shower gels, as well as nickel , should also be avoided at all costs.

This has not been clearly clarified. There is evidence that breastfeeding can reduce the risk of atopic eczema. However, there is no scientific consensus on this. Nevertheless, at least four months of breastfeeding is recommended for atopic diseases.
Cradle cap on the scalp and face can be the first sign of atopic dermatitis in babies. There is also red and scaly eczema on the bends of the arms and legs. The baby is also plagued by agonizing itching which manifests itself in scratching and crying.
If bacteria are responsible for atopic dermatitis in babies, SkinCare Protect can help. SkinCare Sensitive is the perfect moisturizer for skin prone to neurodermatitis.
Certain foods frequently trigger allergic reactions in babies:
Atopic dermatitis is a chronic disease that has not yet been cured and is characterized by severe itching and relapses.
A major factor in atopic dermatitis in babies is that the skin’s protective layer is too weak. SkinCare Protect helps to protect the skin’s protective layer and ensures a balanced skin barrier. However, environmental influences such as animal hair and mites or a generally weakened immune system can also promote atopic dermatitis in babies.
One of the most common skin conditions in babies is atopic dermatitis, also known as neurodermatitis. As children do not understand what is happening to them, neurodermatitis is particularly bad for them. The itching and the associated scratching are also very stressful for children.
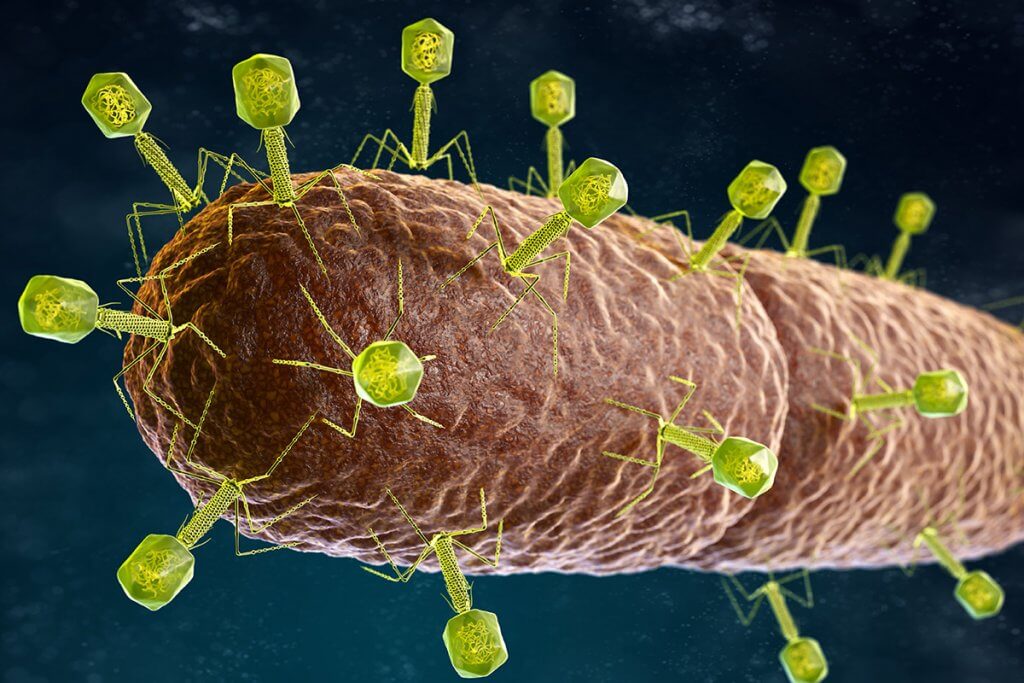
On our skin bacteriophages ensure that the balance of microorganisms is maintained. They are specialized in fighting certain bacteria.
If atopic dermatitis symptoms occur, this is an indication that certain germs are gaining the upper hand and our skin health is at risk.
Staphylococcus aureus is a spherical, gram-positive bacterium that is often responsible for skin problems.
The targeted use of natural phages makes it possible to promote the balance of organisms on the skin. This is a natural way to reduce neurodermatitis.
At Sanubiom, we rely on the use of phages for neurodermatitis, which help to reduce redness and skin irritation. This is how we promote with Sanubiom SkinCare Protect the skin flora. And we restore the balance of the skin’s barrier function in neurodermatitis patients.
SKINCARE PROTECT
Probiotic skin protection SkinCare Protect with Phage Technology.
Your skin comes to rest.
Author: Christian Unterlechner, Dipl.-Ing. (FH), MBA
“From our own experience with neurodermatitis – and the long path of suffering associated with skin conditions like this – we started to look for alternative solutions to drug treatments. We are very happy to share the knowledge and experience that has gone into the years of developing our SkinCare products with you.”
Share post