General
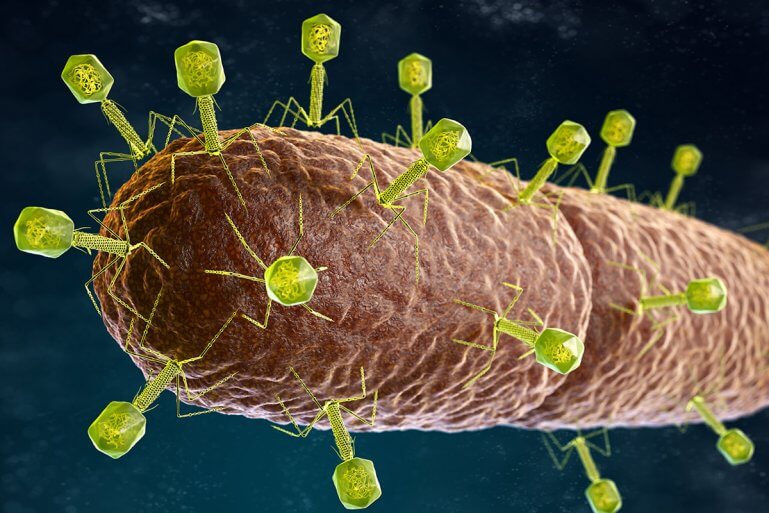
The study investigates how certain strains of Klebsiella pneumoniae (Kp), particularly the Kp2 clade, are associated with the development and exacerbation of inflammatory bowel disease (IBD). Researchers have investigated the use of bacteriophages – viruses that target and kill bacteria – to suppress these pathogenic strains.
Kp strains in IBD: The study found that certain Kp strains, particularly the Kp2 clade, are highly prevalent in patients with IBD. These strains were associated with proinflammatory responses leading to disease flares.
Development of phage therapy: The research team developed a combination of phages that effectively combated the Kp2 strains. Through an iterative process, they selected phages that could not only kill the Kp2 bacteria but also prevent the emergence of resistant strains.
Animal studies: In animal studies on mice, phage treatment significantly reduced inflammation in the colon caused by Kp. The treatment also reduced the bacterial load and improved the survival of the animals.
In a clinical study with healthy adults, the phage combination was administered orally. The study showed that the phages were well tolerated and persisted in the gut. No serious side effects were reported, suggesting that phage therapy may be a viable option for treating bacterial infections associated with IBD.

The researchers developed a bacteriophage combination therapy to combat antibiotic-resistant strains of the Klebsiella pneumoniae (Kp) Kp2 clade associated with inflammatory bowel disease (IBD). An iterative process was used to isolate and test phages that could effectively suppress Kp2 strains. Initially, six phages targeting the Kp-2H7 strain were identified, obtained from wastewater and clinical samples. These phages were tested and resistant Kp2 mutants emerged, leading to further rounds of isolation using the resistant strains as targets. In total, 41 phages were isolated and tested across different Kp2 strains and mutants, resulting in the creation of 18 phage combinations. Of these, only certain combinations were effective in preventing Kp2 regrowth and were selected for further in vivo testing in mice, which showed promising results in reducing bacterial load and preventing resistant strains.

The study highlights the potential of bacteriophage therapy in the treatment of IBD-associated bacterial infections, particularly in relation to the Kp2 clade. The researchers discuss how this therapy could target harmful bacterial strains without affecting the beneficial microbiota, providing a significant advantage over broad-spectrum antibiotics. The results suggest that phage therapy could reduce inflammation and bacterial load in the gut and holds promise as a complementary or alternative treatment to current IBD therapies. However, the researchers emphasize the need for further studies to optimize phage combinations and better understand the long-term effects, especially in humans.
The study shows that phage therapy has great potential for the management of bacterial infections in IBD patients. However, further research is needed to explore the long-term effects and to optimize treatment protocols for wider clinical application. The use of personalized phage treatments tailored to the patient’s bacterial profile could revolutionize the management of chronic diseases such as IBD.